Does Brain Plasticity Increase After a Head Injury?
Medically reviewed by Nancy Hammond, M.D.
By James Roland for healthline.com on July 28, 2022
Brain plasticity, also called neuroplasticity, refers to the brain’s ability to adapt its structure and function in response to changes, such as a head injury or aging. Brain plasticity also involves the formation of new connections between neurons (brain cells).
The brain’s ability to reorganize these features after an injury affects the nature of post-injury recovery.
The severity of the injury goes a long way toward determining how the brain responds. But it’s often possible to boost brain plasticity with interventions and rehabilitation during the healing process.
What is brain plasticity?
Brain plasticity is a term that refers to the brain’s ability to restructure and reconfigure itself in response to change.
Change that can influence the brain comes in several forms. Expected changes include learning, experience, and aging. Unexpected changes include things like stroke and head injury.
Neuroplasticity has long been observed in children. It involves a process called neurogenesis, which is the formation of new neurons in the brain (and elsewhere in the nervous system).
There are two basic types of brain plasticity: structural and functional.
Structural Plasticity
Structural plasticity refers to the way the brain’s physical structure changes in response to learning.
For example, a small 2018 studyTrusted Source showed that healthy adults who participated in balance training twice a week, for 12 weeks, experienced thickening in certain areas of the brain involved in spatial orientation.
A 2016 study examined neuroplasticity in people learning to read Braille. It found that over the course of daily lessons, for 3 weeks, study participants developed increased connectivity in regions of the brain involved in processing sensations like touch.
Functional Plasticity
Functional plasticity refers to the brain’s ability to heal itself after injury. To achieve this, healthy regions of the brain adapt to take over certain functions that the damaged parts of the brain used to perform. This makes functional plasticity especially relevant for people recovering from head injuries.
A 2017 review of studies examining the role of neuroplasticity in stroke recovery found that a stroke can actually trigger neuroplasticity in certain areas. Neuroplasticity plays a role as the brain tries to resume regular functions, like speaking and controlling the movement of limbs.

Can brain plasticity help you heal after a TBI?
A traumatic brain injury (TBI) refers to changes in brain function or brain health caused by an external force, such as a serious blow to the head.
The Centers for Disease Control and Prevention (CDC)Trusted Source reports that there were more than 220,000 TBI-related hospitalizations in 2019 and more than 64,000 TBI-related deaths the following year.
A TBI differs from a nontraumatic brain injury, also known as an acquired brain injury. Acquired brain injuries are those caused by internal factors, such as a stroke, which can damage brain tissue and affect muscle control, speech, cognition, and other functions.
When spontaneous brain plasticity doesn’t occur, it’s sometimes possible to boost neuroplasticity artificially.
A 2020 review of neuroplasticity therapies to treat stroke survivors suggests that approaches such as brain stimulation therapy and virtual reality might help enhance brain plasticity. It may also be possible to transfer nerves from healthy parts of the brain to injured parts.
Similarly, a 2017 review of studies on cognitive rehabilitation following TBI, suggests that memory and other thinking skills may be recovered to some degree with the help of cognitive rehabilitation. The studies showed how cognitive rehabilitation helped to modify damaged neural connections and various brain functions.
Does a brain injury increase neuroplasticity?
Because different regions of the brain are responsible for different functions, the location and severity of an injury determine which functions are affected and to what degree.
For example, certain areas of the brain are responsible for your ability to move certain parts of the body, like your left arm or your right foot.
This is where brain plasticity can help you heal after a brain injury. Just as exercise and learning can enhance brain structure and function, the body’s natural healing and recovery process after an injury can also increase neuroplasticity.
When neurons die due to injury, the brain naturally responds within a few days by developing new neural networks and recruiting various types of cells to take the place of those damaged or killed in the injury.
The extent to which neuroplasticity occurs depends on an individual’s age, the location of the injury, and other factors.
Does age matter after brain injury?
Whether it’s a brain injury or a broken wrist, being younger is always an advantage when it comes to recovery.
A 2008 studyTrusted Source of TBI survivors noted that disability scores following a TBI tended to be significantly better among younger TBI survivors compared with older individuals, even when those older survivors had less severe injuries. And the younger patients improved more in the first 5 years after the injury.
A 2019 report notes that because age affects neuroplasticity, the need for more strategies and therapies to compensate for age-related changes should be a higher priority in the face of an aging population.
Can you see brain plasticity on an MRI?
One of the most useful tools in diagnosing the impact of a TBI, stroke, or other injury or illness affecting the brain is magnetic resonance imaging (MRI).
An MRI can detect many changes in brain structure and function. Current technology is far from perfect, but it’s continuing to improve.
A 2021 articleTrusted Source suggests that advanced MRI techniques are helping doctors develop a more accurate picture of mild TBIs. This may help improve the treatment and understanding of mild TBIs in the future.
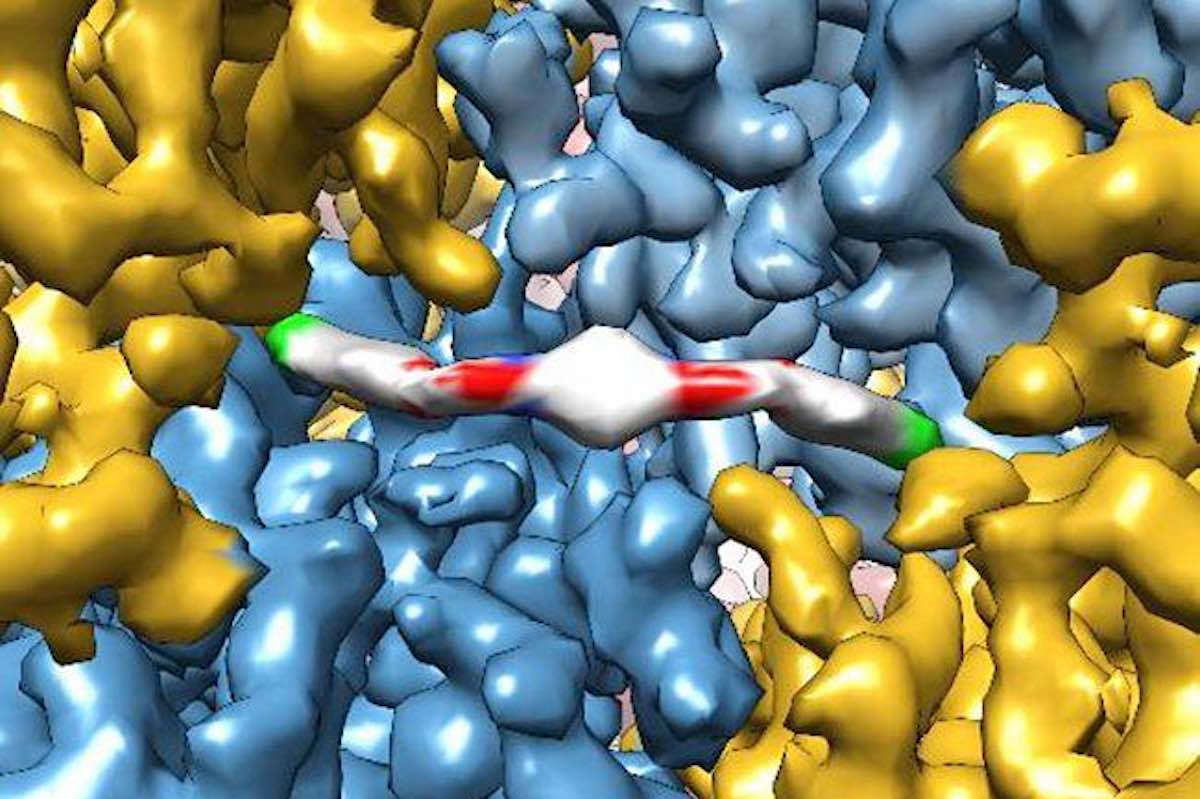
A newer type of MRI, called functional MRI (fMRI), can help doctors observe brain activity, not just brain structure. This may be particularly helpful in studying brain damage and recovery.
A 2017 studyTrusted Source of neuroimaging after TBI notes that fMRI can detect changes in thinking skills, emotions, and the course of neuroplasticity after an injury to the brain. The study says that fMRI is a helpful tool in assessing the damage caused by TBI and tracking brain changes during recovery.
But fMRI, the study says, will need to be accompanied by other data if it’s going to inform treatment decisions. This includes information gathered during cognitive-behavioral evaluations and other assessments.

How long does it take to heal after a TBI?
The time necessary to heal from a TBI can vary considerably from one person to the next. This is based mostly on the seriousness of the injury, as well as its location, the age of the individual, and that person’s overall physical and mental health.
A full recovery from a mild TBI can be expected in about 3 months. People with a moderate TBI will take longer to heal and will typically need cognitive rehabilitation, physical therapy, and other interventions.
Predicting the degree and length of recovery from a severe TBI is very difficult, and should be done on a case-by-case basis.
Takeaway
Brain plasticity after a head injury is when brain functions thought to be lost due to damage begin to be adopted by other, healthy brain tissue.
While not all functions can be reorganized or reestablished completely, the brain’s remarkable adaptability can often help people who had a stroke, traumatic brain injury, or other harmful events recover some function.
Brain plasticity can be encouraged through cognitive therapy, physical therapy, and other treatments.
CLICK HERE to read the original article











 When a person has a stroke, blood flow to the brain is interrupted, causing brain cells to die within minutes due to lack of oxygen. In some cases, this can result in paralysis, speech and language problems, vision problems, and memory loss. But in a new study, researchers have shown that stem cell therapy increases nerve cell production in mice with brain damage due to stroke.
When a person has a stroke, blood flow to the brain is interrupted, causing brain cells to die within minutes due to lack of oxygen. In some cases, this can result in paralysis, speech and language problems, vision problems, and memory loss. But in a new study, researchers have shown that stem cell therapy increases nerve cell production in mice with brain damage due to stroke.