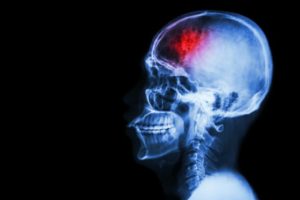
 When a person has a stroke, blood flow to the brain is interrupted, causing brain cells to die within minutes due to lack of oxygen. In some cases, this can result in paralysis, speech and language problems, vision problems, and memory loss. But in a new study, researchers have shown that stem cell therapy increases nerve cell production in mice with brain damage due to stroke.
When a person has a stroke, blood flow to the brain is interrupted, causing brain cells to die within minutes due to lack of oxygen. In some cases, this can result in paralysis, speech and language problems, vision problems, and memory loss. But in a new study, researchers have shown that stem cell therapy increases nerve cell production in mice with brain damage due to stroke.
by Marie Ellis, MedicalNewsToday.com (August 22, 2016) — The researchers – led by Berislav Zlokovic, M.D., Ph.D., from the University of Southern California (USC) – publish their findings in the journal Nature Medicine.
According to the Centers for Disease Control and Prevention (CDC), stroke is the fifth leading cause of death in the United States and is also a major cause of disability in adults.
The effects of a stroke depend on the location of the blockage and how much brain tissue is involved, but a stroke on one side of the brain will result in neurological effects on the opposite side of the body.
For example, a stroke on the right side of the brain could produce paralysis on the left side of the body, and vice versa.
A stroke in the brain stem can affect both sides of the body and could leave the patient in a so-called locked-in state, where the patient is unable to speak or move the body below the neck.
Given that about 800,000 people in the U.S. have a stroke each year, the researchers of this latest study wanted to investigate potential therapies.
Therapy is a combination of two methods
The researchers say their therapy is a combination of two methods. One involves surgically grafting human neural stem cells onto the damaged area, where they are able to mature into neurons and other brain cells.
The other therapy uses a compound called 3K3A-APC, which has been shown to help neural stem cells that have been grown in a petri dish grow into neurons. But the researchers say it was not clear what effect the molecule – called activated protein-C (APC) – would have on live animals.
As such, the team used mice for their experiment, and they found that a month after inducing stroke-like brain damage in the mice, those that had received both the stem cells and 3K3A-APC performed much better on motor and sensory function tests, compared with mice that received only one of the treatments or neither.
The researchers also observed that the mice given 3K3A-APC had more stem cells survive and mature into neurons.
But how did the researchers induce stroke-like brain damage in the mice? They disrupted blood flow to a specific brain area.
Then, 1 week later, which is the mouse equivalent of several months in humans, the researchers inserted the stem cells next to the dead tissue and administered either a placebo or 3K3A-APC.
“When you give these mice 3K3A-APC, it works much better than stem cells alone,” says Dr. Zlokovic. “We showed that 3K3A-APC helps the cells convert into neurons and make structural and functional connections with the host’s nervous system.”
‘No one in the stroke field has ever shown this’
The researchers also looked at the connections between the neurons that grew from the stem cells in the damaged brain region and nerve cells in the primary motor cortex.
The team found that the mice given the stem cells and 3K3A-APC had more neuronal connections – synapses – that linked those areas, compared with the mice given the placebo.
Then, when the researchers stimulated the mice’s paws with a vibration, the neurons that grew from the stem cells exhibited a stronger response in the mice that were treated.
“That means the transplanted cells are being functionally integrated into the host’s brain after treatment with 3K3A-APC. No one in the stroke field has ever shown this, so I believe this is going to be the gold standard for future studies.” ~Dr. Berislav Zlokovic
Following on from this study, the researchers want to pursue another phase II clinical trial to examine whether the treatment combination can encourage the growth of new neurons in human stroke patients to improve function.
They say that if that trial is successful, it could be possible to test the therapy’s effects on other conditions, including spinal cord injuries.
“This USC-led animal study could pave the way for a potential breakthrough in how we treat people who have experienced a stroke,” says Jim Koenig, Ph.D., program director at the National Institute of Health’s National Institute of Neurological Disorders and Stroke (NINDS), who funded the study.
“If the therapy works in humans,” he adds, “it could markedly accelerate the recovery of these patients.”

