Fatigue After Brain Injury
By Katherine Dumsa, OTR/L, CBIS and Angela Spears, MA, CCC-SLP, DPNS, CBIS, Rainbow Rehabilitation Centers
Fatigue is a part of life that is experienced by everyone. Whether it is from a busy day at work, a demanding workout, or after paying attention to a long lecture, the term “I’m tired” is exceedingly common.
Fatigue and Traumatic Brain Injuries
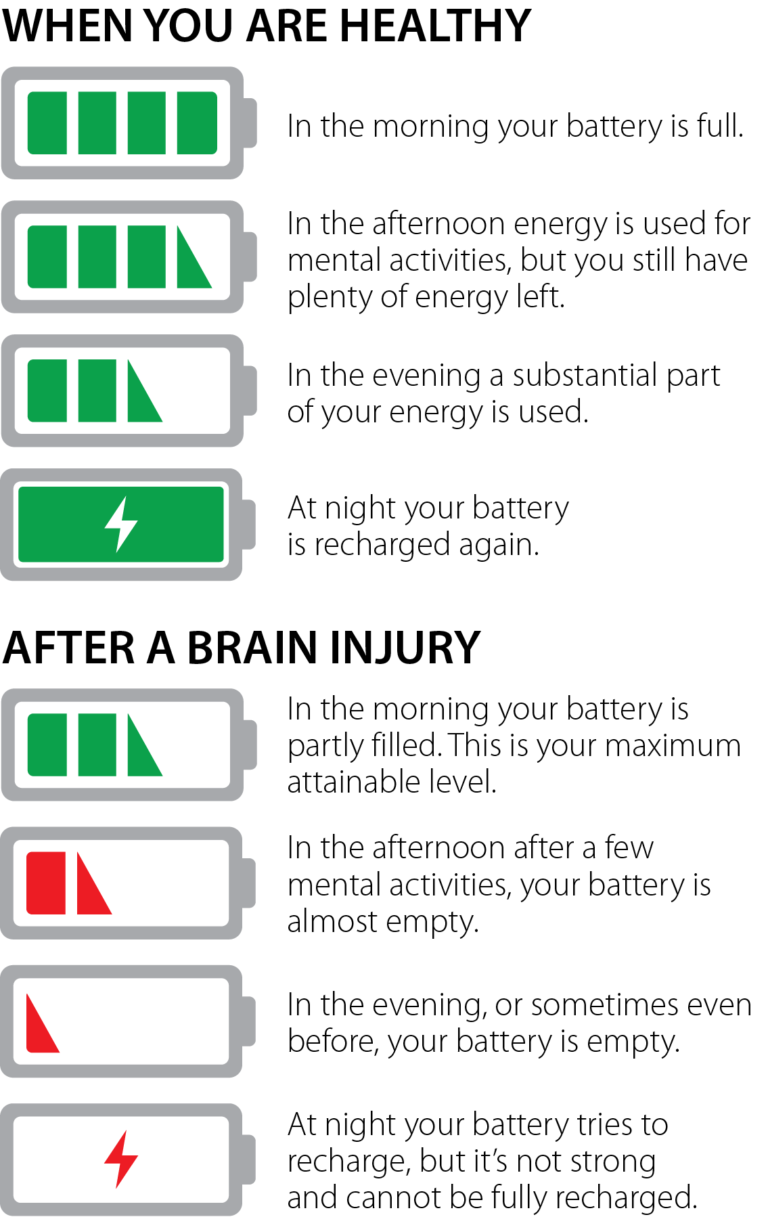
For individuals with brain injuries, fatigue (sometimes referred to as cognitive fatigue, mental fatigue, or neurofatigue), is one of the most common and debilitating symptoms experienced during the recovery process. It can become a significant barrier to one’s ability to participate in the activities they want and need to do in daily life. It is reported that as many as 98% of people who have experienced a traumatic brain injury have some form of fatigue. Many report that fatigue is their most challenging symptom after brain injury. Reasons for the fatigue are not well understood but may include endocrine abnormalities, the need for the brain to work harder to compensate for brain injury deficits (in other words, inefficiency), or changes to brain structures.

Assessment Tools to Determine Fatigue Levels
Fatigue can be difficult to identify because it is not always reported by the patient or obvious to others. Clinicians use various self-report assessment tools to gain further information on a patient’s fatigue levels and the impact it has on their overall daily functioning. Two of the scales specifically designed for individual patients with brain injuries include the Barrow Neurological Institute Fatigue Scale (BNI) and the Cause of Fatigue Questionnaire (COF). Clinicians must also evaluate physical and mental changes, which can lead to depression and other psychiatric conditions following brain injury. The changes can commonly present as overwhelming fatigue.
Symptoms
Generally, those who have sustained brain injuries have described fatigue as a sense of mental or physical tiredness, exhaustion, lack of energy, and/or low vitality. Physical observations of fatigue include yawning, an appearance of confusion or “brain fog,” or easily losing attention and concentration. In more severe cases, it may present as forgetfulness, irritability, slurred speech, or dizziness. Emotions can become raw at this level of fatigue, affecting mood, motivation, and interaction with one’s social network. To manage fatigue effectively, individuals must learn to identify the symptoms of fatigue and how to modify activities that may trigger fatigue. Managing fatigue effectively will help decrease stress levels and improve overall performance for both work and home activities. Some fatigue-inducing activities include:
Symptoms of fatigue can include:
 Fatigue Is Not Laziness
Fatigue Is Not Laziness
In today’s multi-media society, we take in, absorb, and process large amounts of information every day. It can be difficult for family members or peers to understand the limitations caused by fatigue following a brain injury. Unfortunately, it can be mistaken for laziness or an unwillingness to participate in therapies and daily activities. It is important to understand that lacking the mental energy needed to complete tasks does not equate to lacking the desire to complete those tasks. Many individuals struggling with fatigue have motivation but lack the energy to keep up with daily demands.
Coping Strategies Used to Ease Symptoms
When managing fatigue, it is important to identify and treat physical factors that may be contributing to the fatigue. Recognizing early signs of fatigue and working with the patient so they understand how to respond to these is beneficial. By learning to recognize these triggers, one can learn coping strategies to successfully meet daily demands, ultimately increasing quality of life. These strategies include:
Organizing daily activities – Utilize a checklist or planner to set a to-do list. Break up complex projects into manageable tasks. When completing these tasks, minimize environmental stimulation as much as possible.
REFERENCES
This article first appeared in the Summer 2018 issue of Rainbow Visions Magazine available at www.rainbowrehab.com.
CLICK HERE to read the original article